Awareness and Education
So perhaps you’re here because you have a chronic illness, are new to the community and want to learn more.
Or perhaps you’re finding resources to share with friends and family who are coming to terms with learning about chronic illness. Or maybe you simply want to educate yourself about the topic of chronic illness and disability that has never had a good enough 'media representation'.
You can find lots of resources on this page to share with anyone who wants to educate themselves
on chronic illness and disability.
Chronic illness terminology: EXPLAINED
For both awareness and clarity of these terms that are very commonly used, but often misunderstood you can find definitions and explanations here.

There isn’t yet a treatment, cure or remediation that has a consistent and significant efficacy in removal of the condition and return
to normal health

No Cure
An illness or condition that persists for a long time or is constantly recurring. Many chronic illnesses can have no cure, but not all chronic illnesses are incurable.
Chronic

Although a condition or illness can have no cure, there may be management strategies that can alleviate symptoms on a daily basis and improve comfort and quality of life. The combination of strategies used are very unique to each person, and this is due to individual differences.
Management Strategies

Recovery / Remission
Although a condition has no cure, there are cases where people can experience remission or recovery from the symptoms associated with the condition. This means a return to typical health. If a condition is genetic, you may still have the condition, but may have recovered from the symptoms. Recovery / remission can also be temporary or fluctuate at phases throughout a chronic illness.


Healing
Healing is "the process of making or becoming healthy again". Continuous growth and repair happens in our cells every day.
This process could be described as ‘healing’.
If used in chronic illness, we often mean that we are looking to reduce our symptoms and nourish our bodies with a range of 'management strategies' to encourage the growth and repair process. We don’t mean that we are ‘magicking’ our illness or condition away, but simply alleviating symptoms towards recovery or remission.
Things we wish more people understood about chronic illness
-
Our symptoms can fluctuate over the course of our illness
-
We may use mobility aids, supports and other devices on a flexible basis
-
We may not visibly appear "stereotypically unwell"
-
We'd love to attend all plans but sometimes our health takes over
-
The amount of trial and error that goes into finding management strategies to alleviate pain and symptoms wherever possible
-
The perspective changes we have to make to our outlook on our entire lives and future expectations
-
We won't actually often tell you how much pain we're inundated with
-
We may never get fully 'better'
-
We aren't faking being ill, we're faking being well
-
Whilst the severity of our symptoms and manifestation of our condition may change over time it's likely we'll have to manage it forever
-
You'll probably only ever see us on very good days
-
The incessant prejudice and gaslighting we experience due to society's still very ableist perceptions
-
We aren't being lazy. That task or activity will genuinely be detrimental to us
-
How much planning and preparation goes into little things like simply leaving the house for a few hours
-
The physical changes we may have to make to our routines, our careers, our hobbies, our social lives and our homes
-
That our invisible illness isn't so invisible if you look closer into our lifestyle or ask us how we really are or what we deal with, or simply see us on a day that we're using a visible aid or support
Things we have to balance with chronic illness (that you don't always see)

Things to AVOID saying and what to say INSTEAD
Instead of “But you don't look sick/ill/disabled?"
"You look great/happy/healthy/so well but how are you TRULY feeling?"
"I know it's not always visible, could you tell me how your condition affects you?
"You are incredible for what you go through every day, I can't relate but I'm PROUD of you"
"I Googled your condition(s), so I understand a little better, but can you tell me more?"
"Even though I may not fully relate, I'm here to support you"
"I BELIEVE you"
Instead of "get well or get better soon"
“I hope this flare eases up soon”
“I’m thinking of you / sending my love + hugs”
“I hope you find some relief to alleviate your symptoms soon”
“I’m here to support you if you need me or want some [virtual] company”
“I can't imagine how hard this must be”
“You've been through so much + I'm proud of you”
“If you want to chat I'm here”
“Don't forget that resting is productive and please take all the time you need”
Instead of not inviting us because we often can't make it
"I'd love you to come but no pressure if you can't make it"
"These plans aren't very accessible, you're invited but if you can't I'll organise something soon that suits you better"
"If I can do anything to accommodate you let me know!”
"I can come over to you if that helps?"
“What types of plans suit you best and we’ll do more of that!”
"Our plans can be as flexible as possible, if you can't make it we can keep rescheduling"
Instead of "at least it's not ___" and/or giving unsolicited advice (eg. you should try ____ as I heard it cured ____)
"Do you want to tell me more about how it feels to have your condition?"
"What management strategies can you use that helps with daily life?"
"What is the long term prognosis of your condition(s)?"
"How does the condition affect your lifestyle?"
"What does a typical day look like for you?"
"What do you use for pain or symptom relief?
"Is there anything that you've found that helps or are you still trialling?"
Toxic Positivity vs. Genuine Positivity in Chronic illness and Disability

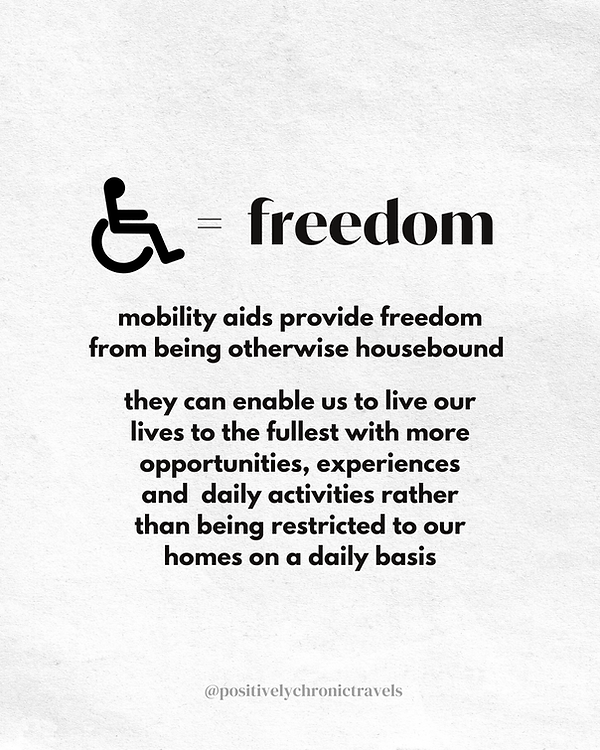
Dynamic Disability and Wheelchair Use
Some disabled people will use a wheelchair on an ‘flexible’ basis. This is known as an 'ambulatory wheelchair user' and means that they may use the aid flexibly around symptoms or flare up but they can still sometimes walk. This can also be known as a Dynamic (variable) Disability.
They may either get up out of the wheelchair and walk as and when tolerated or put down their mobility aid. This is completely valid and should not be questioned!
But if you still want to understand some reasons:
1) to conserve energy and facilitate pacing on days out
or for events
2) to rest any joints or muscles that may be flaring, in pain, inflamed or injured
3) regular episodes of fainting; for example in autonomic dysfunction or for seizures
4) for neurological conditions that affect mobility
5) to leave the house for a task or activity when it otherwise wouldn't be possible without the aid
Does every disabled person have to use a wheelchair to count as disabled?
Some disabled people can't use wheelchairs as they'll actually trigger or worsen symptoms or cause discomfort. Symptom examples include but are not limited to: vertigo, nausea, motion sickness, cervical instability, sciatica, pelvic or spinal instability (partial or full dislocations) which causes pain when seated.
In these cases you likely won't see them mobile unless it's an incredibly good day for symptoms as otherwise they'll be forced to stay home having full rest.
Other factors that can make wheelchair use challenging:
- incomplete level access on your route on public transport
- a big enough car or taxi to store the wheelchair during transport
- if your home isn't level access
- if the location you're going to isn't level access or doesn't have accessible toilets
- if your chair isn't electric or you don't have the funds for one
- if you don't have support from someone to push a manual wheelchair
- if your corridors aren't wide enough
- ableist social perceptions that you're 'giving up' by using a wheelchair
- attitudinal misunderstanding and prejudice about ambulatory mobility aid use
- physical barriers throughout the environment that make wheelchair use complicated or not possible
Flexible Mobility Aid or Support Use
Whilst people who use a wheelchair on a flexible basis but can still walk are known as 'Ambulatory Wheelchair Users', people may also use another type of mobility aid, general aid or support that has an assistive purpose on a flexible basis too. They may identify also as having a Dynamic Disability which is variable and unpredictable.
However there is a common societal misconception that if we take off a support or suddenly stop using a mobility aid, that we are faking it or our condition isn't real. This is an incredibly harmful stereotype and is not the case. Dynamic disability may apply to many conditions that are not immediately obvious or visible and may also therefore be 'invisible illnesses or conditions'.
These aids or supports may just have a specific purpose for a particular symptom and / or situation.
For example:
-
a joint dislocates, is sprained, injured
-
for fatigue, to conserve energy or as assistance when this symptom occurs
-
for joint instability on moving transport where transport can be particularly triggering for pain and symptoms
-
pain levels are high
-
you are able to walk a little but not a lot
-
you have sciatica, back pain or pelvic subluxations and can't sit without this aid
The list could be endless and here are only a few examples to demonstrate that it does not mean anyone is faking it if an aid or support is used in a certain situation or for a specific symptom.
.png)






















.png)